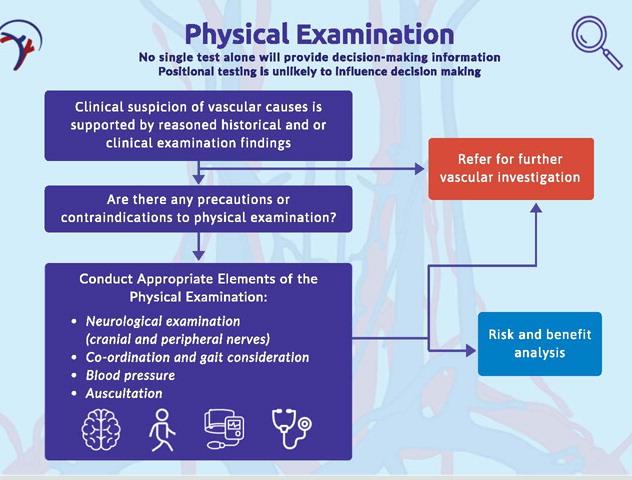
The “International Framework for Examination of the Cervical Region for Potential Vascular Pathologies of the Neck Prior to Musculoskeletal Intervention” provides a comprehensive guide for clinicians to identify and manage vascular pathologies in patients presenting with neck and/or head pain. Developed by the International Federation of Orthopaedic Manipulative Physical Therapists (IFOMPT), this framework is based on contemporary evidence and expert consensus. It emphasizes the importance of thorough patient history, physical examination, and clinical reasoning to differentiate between musculoskeletal disorders and vascular pathologies. Key components include blood pressure measurement, neurological examination, and carotid artery assessment. The framework also highlights the significance of shared decision-making and patient-centered care to ensure safe and effective treatment. This document aims to support clinicians in early identification of vascular issues, thereby improving patient outcomes and minimizing risks associated with musculoskeletal interventions.
The document is a position statement from the International Federation of Orthopaedic Manipulative Physical Therapists (IFOMPT) addressing the assessment of vascular pathologies in the cervical region prior to musculoskeletal interventions.
The distinguishing features of vascular pathologies of the neck include:
1. Symptoms Presentation:
o Headache: Often described as “unusual” or different from typical headaches.
o Neck Pain: Can be severe and progressive.
o Facial Pain: May accompany neck pain.
o Cranial Nerve Dysfunction: Symptoms like ptosis, facial palsy, and Horner’s syndrome.
o Transient Ischemic Attack (TIA) or Stroke: Sudden neurological deficits.
o Visual Disturbances: Such as diplopia or vision loss.
o Dizziness and Disequilibrium: Especially with vertebral artery involvement.
o Nausea and Vomiting: Can occur with severe cases.
o Slurred Speech and Confusion: Indicative of central ischemia.
2. Risk Factors:
o Recent Trauma: History of neck trauma or manipulation.
o Vascular Anomalies: Presence of vascular malformations.
o Cardiovascular Risk Factors: Hypertension, high cholesterol, smoking, and family history of stroke.
o Migraine History: Increased risk of dissection events.
3. Physical Examination Findings:
o Blood Pressure: Elevated readings may indicate acute arterial trauma.
o Neurological Examination: Signs of upper motor neuron lesions or cranial nerve involvement.
o Carotid Artery Examination: Asymmetry in pulse, presence of a pulsatile mass, or bruit on auscultation.
4. Clinical Patterns:
o Dissection Events: Often present with headache, neck pain, visual disturbances, and neurological deficits.
o Nondissection Events: May present with headache, paresthesia, and less commonly, neck pain.
The key risk factors for vascular pathologies of the neck include:
- Recent Trauma:
- History of recent neck or head trauma, such as from a car accident, sports injury, or a fall.
- Vascular Anomalies:
- Presence of congenital or acquired vascular anomalies or malformations.
- Smoking:
- Current or past smoking history.
- Migraine:
- History of migraines or severe headaches.
- High Cholesterol:
- Elevated total cholesterol levels.
- Recent Infection:
- Recent infections that may contribute to vascular inflammation or dysfunction.
- Hypertension:
- High blood pressure, which increases the risk of vascular events.
- Oral Contraception:
- Use of oral contraceptives, which can increase the risk of vascular events in some individuals.
- Family History of Stroke:
- Family history of stroke or other vascular diseases.
These risk factors should be thoroughly considered during patient history taking to assess the potential for vascular pathologies and guide appropriate clinical decision-making.
The clinical features of dissection and nondissection vascular events can differ significantly. Here are the key differences:
Dissection Events:
- Headache:
- Commonly reported in 81% of cases.
- Often described as sudden and severe, sometimes referred to as a “thunderclap” headache.
- Neck Pain:
- Reported in 57-80% of cases.
- Typically localized to the side of the dissection.
- Visual Disturbance:
- Occurs in about 34% of cases.
- May include double vision or transient vision loss.
- Paresthesia (Upper Limb):
- Reported in 34% of cases.
- Sensation of tingling or numbness in the upper limb.
- Dizziness:
- Occurs in 32% of cases.
- May be associated with vertigo or a sense of imbalance.
- Paresthesia (Face):
- Reported in 30% of cases.
- Tingling or numbness in the facial area.