Eswt tendons systematic reviewEswt tendons systematic review
Shock wave therapy (ESWT) was first used for kidney stones, as a method to disintegrate them (1). At the beginning of the 1990s, it was used as a non‑invasive procedure to successfully treat calcific tendinitis. From then on, further tendon disorders were effectively addressed, with subsequent research work on their biological and clinical effects. Basically, there are two types of ESWT: Focused and radial shockwave therapy. Focused ESWT is extensively used in clinical practice; it comprises high‑energy pressure pulses that converge to a focal point, where maximal pressure is reached. They have an initial high positive pressure wave (up to 80 MPa) with a rapid raise time (30‑120 nsec), followed by a negative wave (5‑10 MPa). The pulse duration is short, 5 µsec (2).
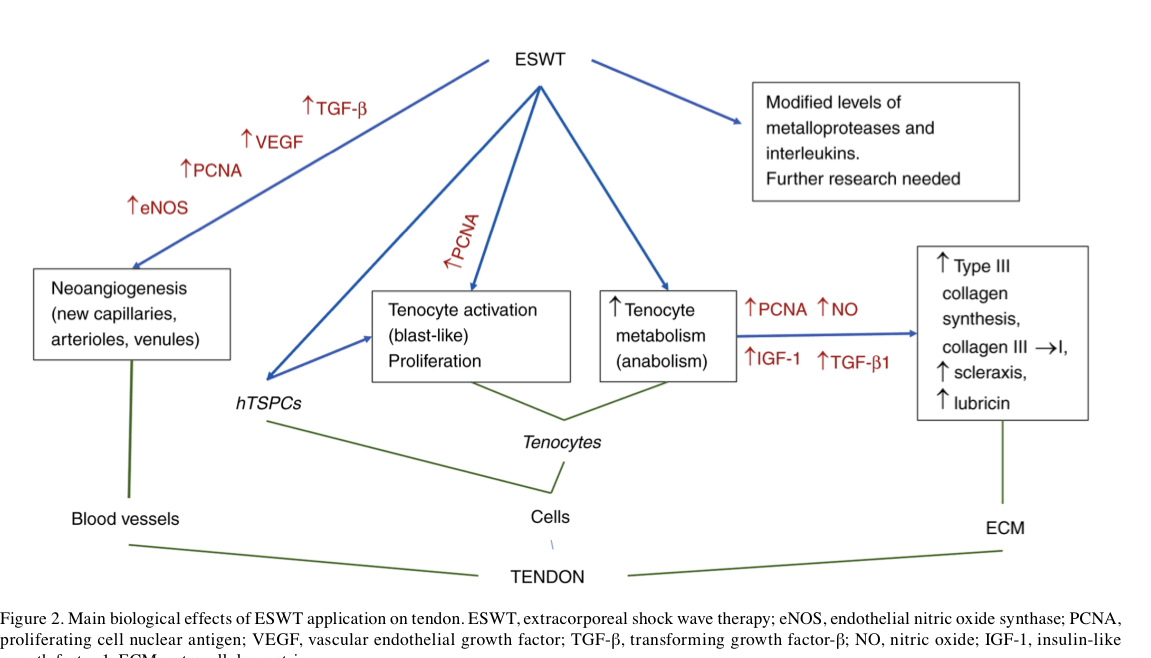
Wave energy is released at tissue interfaces that have different acoustic impedances, causing compressive and shear loads. Microscopic gas bubbles develop and collapse in the interstitial fluid of tissues, a phenomenon called cavitation. It produces high localized stresses, a mechanical stimulation (3). Radial ESWT is characterized by a diverging pressure field, with a maximal pressure at the source (4). Certain researchers agree that radial ESWT cannot be described as real extracorporeal shockwaves as they lack their physical features and proposed to name them radial pressure wave therapy, as a distinct form of therapy (5). Energy flux density (EFD) determines the energy flow through an area perpendicular to the direction of wave propa‑ gation and its units are mJ/mm2. The classification of ESWT includes low (<0.08 mJ/mm2), medium (<0.28 mJ/mm2) and high (<0.60 mJ/mm2) EFD (6). Microscopically, tendons are composed of cells, tenocytes and extracellular matrix (ECM) that contains collagen, elastin and ground substance. Tenocytes, spindle‑shaped cells, are responsible for matrix maintenance and repair and occupy 5% of the tissue volume. ECM contains mainly type I collagen, while type III collagen is the next‑most abundant and critical in pathologic tendons and tendon‑healing processes (7). Tenocytes may convert mechanical stimulation into a biochemical response, leading to the release of growth factors and cellular adaptation (8). The process is known as mecha‑ notransduction and may lead to maintenance, remodeling or degeneration of the tendon through regulation of anabolic and catabolic genes. The mechanisms of action remain to be fully elucidated. The therapeutic field of ESWT is continuously expanding, as research adds new opportunities. Post‑stroke spasticity was addressed with comparable efficacity with botulinum toxin and both types of ESWT, with the radial form providing the best short‑ and medium‑term results (9).
Materials and methods
A comprehensive literature search was performed in the online databases PubMed (https://pubmed.ncbi.nlm.nih.gov/) and Cochrane Library (https://www.cochrane.org/Both) using combinations of the following key words: ‘extracorporeal shockwave therapy’, ‘biological effect’ and ‘tendon’. through. The search included papers available as an abstract since 1988
Biological effects of extracorporeal shockwave therapy in tendons: A systematic review
DANIELA POENARU1, MIRUNA IOANA SANDULESCU2 and DELIA CINTEZA1
1Department of Rehabilitation, Carol Davila University of Medicine and Pharmacy; 2Doctoral School, Clinical Pharmacology, Carol Davila University of Medicine and Pharmacy, 020021 Bucharest, Romania
Received September 24, 2022; Accepted November 30, 2022
DOI: 10.3892/br.2